Medical Devices Reimbursement Market Statistics 2025 Analysis By Application (Hospitals, Outpatient facilities), By Type (Pbulic Reimbursement, Private Reimbursement), and By Region (North America, Latin America, Europe, Asia Pacific, Middle East, and Africa) - Size, Share, Outlook, and Forecast 2025 to 2032 (Financial Impact Analysis)
ID : MRU_ 395166 | Date : May, 2025 | Pages : 340 | Region : Global | Publisher : MRU
Introduction:
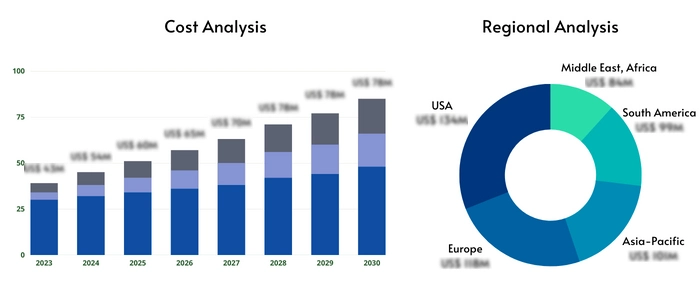
The Medical Devices Reimbursement Market is poised for significant growth from 2025 to 2032, projected at a CAGR of 8% (example CAGR). This expansion is driven by several key factors. Firstly, the aging global population necessitates increased healthcare expenditure, leading to a higher demand for medical devices and consequently, a larger reimbursement market. Technological advancements, such as the development of minimally invasive surgical devices, advanced diagnostic tools, and personalized medicine technologies, are further fueling this growth. These innovations often come with higher costs, impacting the reimbursement landscape and necessitating sophisticated reimbursement models. The market also plays a crucial role in addressing global challenges. Efficient reimbursement systems ensure accessibility to life-saving medical technologies, reducing health disparities and improving overall population health outcomes. The increasing prevalence of chronic diseases like diabetes, cardiovascular ailments, and cancer, alongside the rising incidence of accidents and trauma, places a strain on healthcare systems worldwide. A well-functioning reimbursement mechanism is vital to alleviate this pressure, allowing for timely access to essential medical devices without creating an undue financial burden on patients or healthcare providers. Moreover, the integration of digital health technologies, such as telehealth and remote patient monitoring, is transforming the delivery of healthcare and influencing the reimbursement models. These technologies often require unique reimbursement strategies to incentivize their adoption and maximize their impact on patient care. Finally, the growing focus on value-based healthcare, which emphasizes the quality and outcomes of care rather than just the quantity of services, is impacting how medical devices are reimbursed. The industry is moving towards models that reward effective treatments and better patient outcomes, encouraging innovation and efficiency in medical device development and usage.
The Medical Devices Reimbursement Market is poised for significant growth from 2025 to 2032, projected at a CAGR of 8%
Market Scope and Overview:
The Medical Devices Reimbursement Market encompasses the financial mechanisms and processes involved in covering the costs of medical devices used in healthcare settings. This includes the various types of reimbursement schemes, the entities involved (payers, providers, manufacturers), and the regulations governing these processes. The markets scope extends across diverse technologies, including implantable devices (pacemakers, artificial joints), diagnostic imaging equipment (MRI, CT scanners), therapeutic devices (dialysis machines, ventilators), and numerous other medical technologies. Applications span hospitals, outpatient clinics, ambulatory surgical centers, and even home healthcare settings. The market serves a broad range of industries, including healthcare providers, medical device manufacturers, insurance companies, and government agencies. In the broader context of global trends, this market is intrinsically linked to the rising healthcare expenditure globally. As healthcare systems grapple with rising costs and aging populations, efficient and equitable reimbursement models become increasingly critical. Global trends like the increasing prevalence of chronic diseases, technological advancements in medical devices, and the shift towards value-based care significantly influence the dynamics of this market. The markets ability to adapt to these trends is essential for ensuring sustainable healthcare access and affordability. Furthermore, the markets role in influencing healthcare policy and innovation is vital. effective reimbursement structures encourage development and adoption of innovative medical technologies that ultimately benefit patients. The integration of data analytics and AI is further shaping the market by providing better tools for risk assessment, fraud detection, and more precise cost estimation in reimbursement processes.
Definition of Market
The Medical Devices Reimbursement Market refers to the complete ecosystem surrounding the financial processes for covering the costs of medical devices. This includes the range of products, services, and systems enabling the transfer of funds from payers (insurance companies, government programs, private individuals) to providers (hospitals, clinics) for the use of medical devices. Components include public and private reimbursement schemes, claim processing systems, coding and billing procedures, regulatory compliance measures, and the various contracts and agreements between stakeholders. Key terms in this market include: Reimbursement: The process of receiving payment for medical devices. Payer: The entity providing financial coverage (e.g., Medicare, Medicaid, private insurers). Provider: The healthcare facility or professional using the medical device. Claim: A formal request for payment. Coding: Assigning standardized codes to medical devices and procedures to facilitate billing. Billing: The process of submitting claims to payers. DRG (Diagnosis-Related Group): A classification system used for inpatient hospital reimbursement. APC (Ambulatory Payment Classification): A classification system used for outpatient hospital reimbursement. CPT (Current Procedural Terminology): Codes used for describing medical procedures. HCPCS (Healthcare Common Procedure Coding System): A coding system for healthcare products and services. Bundled Payments: A payment model that combines multiple services into a single payment. Value-Based Reimbursement: Payment models that tie reimbursement to the quality and outcomes of care. Understanding these terms is crucial for navigating the complexities of the medical devices reimbursement market.
Market Segmentation:
The Medical Devices Reimbursement Market can be segmented by type of reimbursement, application, and end-user. These segments are interconnected and influence each others growth trajectories. A comprehensive understanding of each segment is vital for effective market analysis and strategic planning. The interplay between these segments reflects the diverse stakeholders and processes involved in medical device reimbursement.
By Type
Public Reimbursement: This segment encompasses government-funded programs such as Medicare and Medicaid in the US, the National Health Service (NHS) in the UK, and similar programs worldwide. These programs set specific reimbursement rates and criteria for medical devices, often focusing on cost-effectiveness and ensuring equitable access to healthcare. The regulations and procedures governing public reimbursement are typically complex and subject to frequent changes, impacting market dynamics. Public reimbursement often plays a significant role in determining the overall market size and influencing the adoption of certain medical devices.
Private Reimbursement: This segment covers reimbursement from private health insurance companies. These companies operate under different policies and reimbursement structures, leading to variations in coverage and payment rates. Negotiations between device manufacturers, providers, and private insurers significantly influence the pricing and availability of medical devices in the private reimbursement segment. The competitiveness of private insurers and the varying levels of coverage offered impact the affordability and accessibility of medical devices for patients.
By Application
Hospitals: Hospitals represent a major segment, with complex reimbursement procedures involving DRGs, APCs, and other payment models. Hospital reimbursement often depends on the type of procedure, the patients diagnosis, and the length of stay. The regulatory landscape in hospitals is particularly stringent, impacting the reimbursement processes. The size and complexity of hospital systems vary significantly across regions, influencing the dynamics of the reimbursement market.
Outpatient Facilities: This segment includes ambulatory surgical centers, clinics, and other facilities providing outpatient care. Reimbursement in this segment is typically based on APCs or other fee-for-service models. The increasing shift towards outpatient procedures influences the growth of this segment, driving innovation and competition in outpatient medical device reimbursement.
By End User
Governments play a vital role as regulators, payers (through public health programs), and purchasers of medical devices. Government policies, regulations, and budget allocations directly influence market dynamics. Their influence extends to setting reimbursement rates, enforcing quality standards, and shaping healthcare policy, ultimately affecting market access and pricing.
Businesses, primarily healthcare providers and medical device manufacturers, are key players. Providers reimbursement income directly influences their device purchasing decisions. Manufacturers actively engage with payers to secure favorable reimbursement policies for their products. The relationship between these two parties is vital for market growth and innovation.
Individuals, as patients, are the ultimate beneficiaries of the medical devices reimbursement market. Their ability to access needed devices depends on the affordability of these devices and their health insurance coverage. Patient cost-sharing and out-of-pocket expenses significantly impact their choices and access to care.
Market Outlook and Projections:
| Report Attributes | Report Details |
| Base year | 2024 |
| Forecast year | 2025-2032 |
| CAGR % | 8 |
| Segments Covered | Key Players, Types, Applications, End-Users, and more |
| Major Players | Aviva, Nippon Life Insurance, WellCare Health Plans, BNP Paribas, CVS Health |
| Types | Pbulic Reimbursement, Private Reimbursement |
| Applications | Hospitals, Outpatient facilities |
| Industry Coverage | Total Revenue Forecast, Company Ranking and Market Share, Regional Competitive Landscape, Growth Factors, New Trends, Business Strategies, and more |
| Region Analysis | North America, Europe, Asia Pacific, Latin America, Middle East and Africa |
The Top Key Market Players for Medical Devices Reimbursement Market Listed are:
Aviva
Nippon Life Insurance
WellCare Health Plans
BNP Paribas
CVS Health
Market Drivers:
Several factors drive growth in the Medical Devices Reimbursement Market: The aging global population leads to a greater demand for medical devices, increasing the need for reimbursement. Technological advancements result in new and expensive devices requiring robust reimbursement models. Government policies, such as value-based care initiatives, incentivize efficient reimbursement structures. Increasing demand for sustainability pushes for cost-effective solutions and efficient reimbursement strategies. Rising prevalence of chronic diseases necessitates greater access to medical devices, putting pressure on reimbursement systems.
Market Restraints
Challenges include high initial costs of advanced medical devices, creating reimbursement hurdles. Geographic limitations and variations in healthcare systems lead to disparities in reimbursement rates and access. Regulatory complexities and bureaucratic procedures can delay reimbursements, affecting providers and manufacturers. Fraud and abuse in the reimbursement system erode efficiency and increase costs. Data management and interoperability issues hinder the development of efficient reimbursement systems. Variations in insurance coverage across different countries and regions impact market accessibility and affordability.
Market Opportunities
Opportunities include developing innovative reimbursement models aligned with value-based care. Leveraging technology, such as AI and data analytics, to streamline claim processing and reduce fraud. Improving data interoperability to facilitate more efficient reimbursement processes. Expanding coverage of medical devices to underserved populations. Focusing on preventative care and chronic disease management to reduce overall healthcare costs. Promoting partnerships between payers, providers, and manufacturers to develop cost-effective reimbursement models.
Market Challenges
The Medical Devices Reimbursement Market faces significant challenges. Firstly, the escalating cost of innovative medical devices poses a considerable burden on healthcare systems. Balancing the need for advanced technologies with the affordability of reimbursement remains a key challenge. Secondly, the complexity and fragmentation of the healthcare system create significant administrative hurdles. Differing reimbursement policies across various payers (public and private) necessitate intricate navigation and coordination, leading to delays and inefficiencies. Thirdly, ensuring equitable access to medical devices for all populations, regardless of socioeconomic status or geographic location, presents a significant challenge. Disparities in access highlight the need for well-designed reimbursement strategies to address these inequities. Fourthly, preventing fraud and abuse within the reimbursement system requires robust monitoring and regulatory mechanisms. The potential for fraudulent claims and wasteful spending necessitates ongoing efforts to strengthen oversight and accountability. Fifthly, keeping pace with technological advancements and integrating new devices into existing reimbursement models poses ongoing challenges. The rapid pace of innovation requires flexible and adaptable reimbursement frameworks to accommodate new technologies effectively. Sixthly, data management and interoperability across different healthcare systems remain a substantial hurdle. The lack of seamless data exchange between providers, payers, and manufacturers impedes efficient claim processing and creates opportunities for errors and delays. Finally, international variations in reimbursement policies and regulations create complex challenges for medical device manufacturers seeking global market access. Navigating differing regulatory landscapes adds considerable complexity to market expansion strategies.
Market Key Trends
Key trends include a shift toward value-based reimbursement, incentivizing quality over quantity. Increasing adoption of telehealth and remote patient monitoring impacts reimbursement strategies. Growing use of big data and AI for improved claim processing and fraud detection. Emphasis on bundled payments and outcome-based reimbursement models. Expansion of coverage for innovative medical devices through alternative payment models. Development of transparent and patient-centric reimbursement processes.
Market Regional Analysis
North America holds a significant market share due to high healthcare expenditure and advanced medical technology adoption. However, rising healthcare costs and increasing scrutiny of reimbursement practices present challenges. Europe exhibits a mature market with established reimbursement systems, but variations across countries impact market dynamics. Asia Pacific demonstrates rapid growth driven by rising healthcare expenditure and a growing middle class. However, infrastructural limitations and varying regulatory frameworks create opportunities and challenges. Latin America and the Middle East and Africa present emerging markets with significant growth potential but face challenges related to healthcare infrastructure and affordability. Each region presents unique opportunities and challenges regarding regulatory frameworks, healthcare infrastructure, and patient access. The level of technological advancement and integration of digital health technologies influence the efficiency and sophistication of reimbursement systems. The prevalence of chronic diseases and aging populations play a significant role in shaping the demand for medical devices and, consequently, the volume of reimbursements. Political and economic stability also influence the investment in healthcare infrastructure and the implementation of effective reimbursement mechanisms.
Regional Analysis For Medical Devices Reimbursement Market
- United States, Canada, and Mexico Germany, France, UK, Russia, and Italy China, Japan, Korea, India, and Southeast Asia Brazil, Argentina, Colombia Middle East and Africa
Frequently Asked Questions:
What is the projected growth of the Medical Devices Reimbursement Market?
The Medical Devices Reimbursement Market is projected to grow at a CAGR of 8% (example) from 2025 to 2032.
What are the key trends shaping this market?
Key trends include value-based reimbursement, telehealth integration, big data analytics, bundled payments, and improved patient access.
What are the most popular types of medical device reimbursement?
Public and private reimbursement schemes are the most prevalent, with variations across regions and healthcare systems.
What are the major challenges faced by this market?
Challenges include high device costs, administrative complexities, ensuring equitable access, preventing fraud, and adapting to technological advancements.
What are the future growth prospects for this market?
Future growth hinges on adapting to evolving healthcare needs, technological innovations, and improved regulatory frameworks.
Research Methodology
The Market Research Update offers technology-driven solutions and its full integration in the research process to be skilled at every step. We use diverse assets to produce the best results for our clients. The success of a research project is completely reliant on the research process adopted by the company. Market Research Update assists its clients to recognize opportunities by examining the global market and offering economic insights. We are proud of our extensive coverage that encompasses the understanding of numerous major industry domains.
Market Research Update provide consistency in our research report, also we provide on the part of the analysis of forecast across a gamut of coverage geographies and coverage. The research teams carry out primary and secondary research to implement and design the data collection procedure. The research team then analyzes data about the latest trends and major issues in reference to each industry and country. This helps to determine the anticipated market-related procedures in the future. The company offers technology-driven solutions and its full incorporation in the research method to be skilled at each step.
The Company's Research Process Has the Following Advantages:
- Information Procurement
The step comprises the procurement of market-related information or data via different methodologies & sources.
- Information Investigation
This step comprises the mapping and investigation of all the information procured from the earlier step. It also includes the analysis of data differences observed across numerous data sources.
- Highly Authentic Source
We offer highly authentic information from numerous sources. To fulfills the client’s requirement.
- Market Formulation
This step entails the placement of data points at suitable market spaces in an effort to assume possible conclusions. Analyst viewpoint and subject matter specialist based examining the form of market sizing also plays an essential role in this step.
- Validation & Publishing of Information
Validation is a significant step in the procedure. Validation via an intricately designed procedure assists us to conclude data-points to be used for final calculations.
Request Free Sample:
Related Reports


We're cost-effective and Offered Best services:
We are flexible and responsive startup research firm. We adapt as your research requires change, with cost-effectiveness and highly researched report that larger companies can't match.

Information Safety
Market Research Update ensure that we deliver best reports. We care about the confidential and personal information quality, safety, of reports. We use Authorize secure payment process.

We Are Committed to Quality and Deadlines
We offer quality of reports within deadlines. We've worked hard to find the best ways to offer our customers results-oriented and process driven consulting services.

Our Remarkable Track Record
We concentrate on developing lasting and strong client relationship. At present, we hold numerous preferred relationships with industry leading firms that have relied on us constantly for their research requirements.

Best Service Assured
Buy reports from our executives that best suits your need and helps you stay ahead of the competition.

Customized Research Reports
Our research services are custom-made especially to you and your firm in order to discover practical growth recommendations and strategies. We don't stick to a one size fits all strategy. We appreciate that your business has particular research necessities.

Service Assurance
At Market Research Update, we are dedicated to offer the best probable recommendations and service to all our clients. You will be able to speak to experienced analyst who will be aware of your research requirements precisely.
The content of the report is always up to the mark. Good to see speakers from expertise authorities.
Privacy requested , Managing Director
A lot of unique and interesting topics which are described in good manner.
Privacy requested, President
Well researched, expertise analysts, well organized, concrete and current topics delivered in time.
Privacy requested, Development Manager