Clinical Documentation Improvement Market Size By Region (North America, Europe, Asia-Pacific, Latin America, Middle East and Africa), By Statistics, Trends, Outlook and Forecast 2025 to 2032 (Financial Impact Analysis)
ID : MRU_ 427628 | Date : Oct, 2025 | Pages : 241 | Region : Global | Publisher : MRU
Clinical Documentation Improvement Market Size
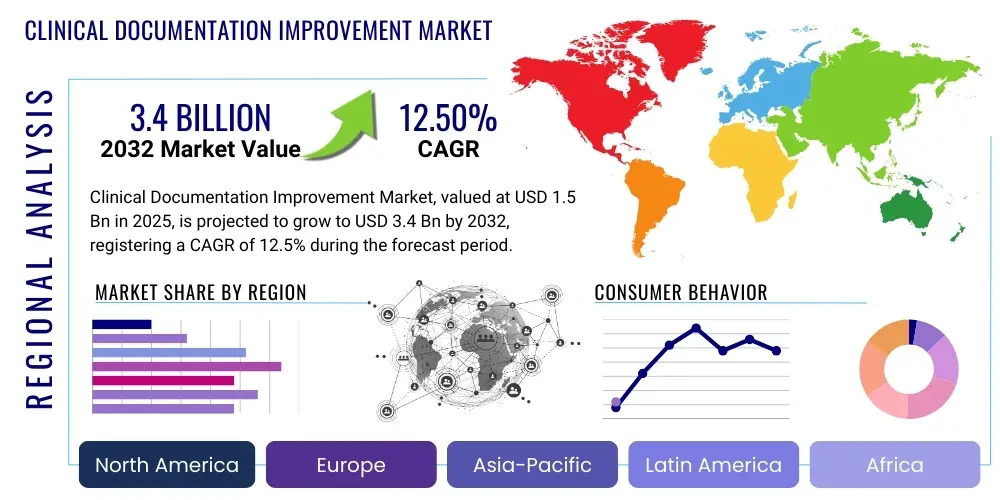
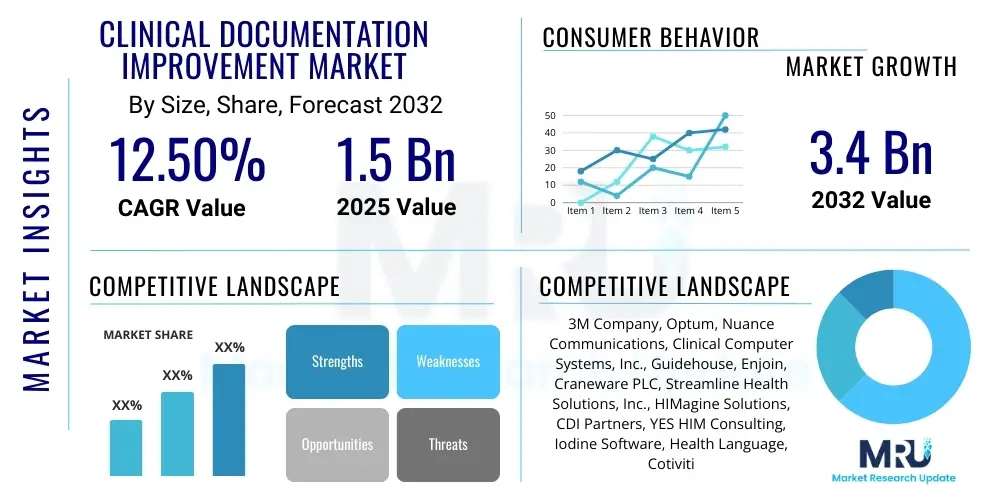
The Clinical Documentation Improvement Market is projected to grow at a Compound Annual Growth Rate (CAGR) of 12.5% between 2025 and 2032. The market is estimated at USD 1.5 billion in 2025 and is projected to reach USD 3.4 billion by the end of the forecast period in 2032.
Clinical Documentation Improvement Market introduction
The Clinical Documentation Improvement (CDI) market encompasses a specialized suite of solutions and services strategically designed to enhance the accuracy, completeness, and consistency of clinical documentation within healthcare organizations. This critical process ensures that medical records precisely reflect the true severity of illness, the complexity of care provided, and the actual resource consumption for each patient encounter. CDI programs leverage a multi-faceted approach, integrating expert chart review by credentialed professionals, targeted education for healthcare providers, and sophisticated technological tools to achieve their objectives. The overarching goal is to transform raw clinical notes into robust, defensible documentation that supports high-quality patient care and optimizes operational efficiency.
Major applications of CDI extend across various facets of healthcare operations. Foremost among these is the improvement of revenue cycle management, where accurate documentation directly translates into optimized and legitimate reimbursement from payers, significantly reducing the potential for claim denials and audit risks. CDI also plays a pivotal role in supporting robust risk adjustment models, which are essential in value-based care frameworks for fair assessment of patient populations and provider performance. Furthermore, these initiatives are indispensable for enhancing compliance with an increasingly complex web of regulatory standards, such as ICD-10 coding guidelines and other evolving mandates from governmental and accreditation bodies. The benefits derived from well-implemented CDI programs are profound and far-reaching, encompassing not only financial gains but also enhanced patient safety through clearer communication and improved quality metrics that contribute to a hospitals reputation and standing.
The markets sustained growth is primarily propelled by several significant driving factors. The escalating complexity of healthcare regulations and coding systems, coupled with the global shift from fee-for-service to value-based care models, mandates meticulous documentation for appropriate resource allocation and quality measurement. There is an increasing imperative for accurate patient data to fuel advanced analytics, critical for population health management, research, and strategic decision-making. Moreover, persistent financial pressures on healthcare providers to maximize legitimate revenue, minimize operational costs, and reduce audit liabilities are compelling organizations to invest in sophisticated CDI solutions. The continuous evolution of Electronic Health Record (EHR) systems also creates a fertile ground for CDI tools that integrate seamlessly, further streamlining the documentation process and enhancing overall data integrity.
Clinical Documentation Improvement Market Executive Summary
The Clinical Documentation Improvement (CDI) market is poised for substantial growth, reflecting its indispensable role in the modern healthcare ecosystem. Current business trends highlight a significant pivot towards integrating advanced technologies, particularly artificial intelligence (AI) and natural language processing (NLP), into CDI workflows. This evolution is transforming CDI from a predominantly manual review process to one that is more proactive, predictive, and data-driven, enabling healthcare organizations to address documentation deficiencies with greater efficiency and precision. The increasing adoption of value-based care models globally is a primary catalyst, as accurate and comprehensive clinical documentation is foundational for demonstrating quality outcomes, managing patient risk, and securing appropriate reimbursement. This strategic importance positions CDI as a critical investment for sustainable healthcare operations.
Regional trends indicate North Americas continued dominance in the CDI market, attributed to its advanced healthcare infrastructure, the early and widespread adoption of electronic health records (EHRs), and a highly complex, regulated reimbursement environment that necessitates robust documentation. Europe is also experiencing steady growth, driven by digital transformation initiatives in healthcare and a collective effort to standardize clinical data across diverse national health systems. Concurrently, the Asia-Pacific region is emerging as a high-growth market, spurred by rising healthcare expenditures, increasing awareness of CDI benefits, and the modernization of healthcare facilities in developing economies. These regional dynamics underscore a global recognition of CDIs value in enhancing both clinical and financial performance.
Segmentation trends within the CDI market reveal a strong preference for integrated software solutions that offer comprehensive capabilities, ranging from automated chart review to real-time provider prompts. Consulting and education services remain crucial, as healthcare organizations often require expert guidance for program implementation, staff training, and ongoing optimization. The deployment model segment shows a growing inclination towards cloud-based solutions due to their inherent scalability, flexibility, and reduced need for on-premise IT infrastructure, particularly attractive to smaller institutions and those seeking rapid deployment. End-user demand is predominantly from hospitals and large health systems, but there is an expanding uptake from ambulatory care centers and physician practices, driven by the broad applicability of CDI across various care settings and its crucial role in managing population health and risk adjustment.
AI Impact Analysis on Clinical Documentation Improvement Market
Common user questions about AIs impact on Clinical Documentation Improvement (CDI) frequently revolve around automation capabilities, accuracy improvements, and the potential for job augmentation rather than displacement for CDI specialists. Users actively seek to understand how AI can streamline the initial phases of chart review, proactively identify potential documentation gaps, and offer real-time, evidence-based suggestions to clinicians, thereby reducing the manual burden and enhancing efficiency. Concerns often include the reliability and interpretability of AI algorithms in highly complex and nuanced clinical scenarios, ensuring data privacy and security, and addressing the ethical implications of AI-driven insights. Expectations are high for AI to not only improve the overall quality and completeness of patient records but also to provide more precise data for analytics, support robust risk adjustment, and integrate seamlessly with existing Electronic Health Record (EHR) systems, ultimately optimizing the entire revenue cycle management process.
- Enhanced efficiency in identifying documentation gaps and discrepancies through automated, intelligent chart review.
- Provision of real-time clinical documentation prompts and alerts directly to healthcare providers, fostering accuracy at the point of care.
- Improved data extraction and sophisticated analysis from vast amounts of unstructured clinical notes utilizing advanced Natural Language Processing (NLP).
- Implementation of predictive analytics to proactively anticipate potential documentation issues, identify opportunities for risk adjustment, and prevent future compliance challenges.
- Automation of routine and repetitive CDI tasks, thereby enabling human specialists to allocate their expertise towards more complex cases, critical thinking, and targeted provider education.
- Attainment of greater consistency, standardization, and adherence to best practices in documentation across diverse healthcare systems and individual clinicians.
- Potential for significantly reduced audit risks, improved financial integrity, and enhanced compliance with a rapidly evolving landscape of regulatory standards and payer requirements.
- Accelerated learning curves for new CDI specialists through AI-powered training modules, decision support systems, and knowledge repositories.
- Seamless and intuitive integration with existing Electronic Health Records (EHRs) and other healthcare IT systems for a unified user experience and comprehensive data flow.
- Generation of advanced insights into physician documentation patterns, enabling healthcare organizations to tailor educational interventions more effectively and foster continuous improvement.
DRO & Impact Forces Of Clinical Documentation Improvement Market
The Clinical Documentation Improvement (CDI) market is propelled by a dynamic interplay of powerful drivers, prominent among which is the escalating complexity of healthcare coding systems, particularly the transition and ongoing updates to ICD-10-CM/PCS. This complexity necessitates meticulous documentation to ensure accurate code assignment, which directly impacts reimbursement and data integrity. Furthermore, the pervasive global transition towards value-based care (VBC) models fundamentally alters how healthcare providers are compensated, tying payments to patient outcomes and quality metrics. In this environment, precise and comprehensive documentation becomes paramount for demonstrating the true burden of illness, the effectiveness of interventions, and overall quality performance. The increasing imperative for accurate, high-quality patient data to support robust clinical analytics, facilitate population health management, and inform strategic decision-making also acts as a significant market driver. These factors collectively create an undeniable need for sophisticated CDI solutions to navigate the modern healthcare landscape effectively.
Despite these strong drivers, the CDI market faces several notable restraints that temper its growth trajectory. The substantial initial investment required for implementing advanced CDI software platforms and comprehensive staff training programs can be a significant barrier for smaller healthcare organizations or those with limited capital. A persistent challenge remains in achieving consistent and robust physician engagement and buy-in, as clinicians often perceive CDI efforts as an added administrative burden rather than a collaborative process. The scarcity of highly skilled and experienced CDI professionals, possessing both clinical knowledge and coding expertise, presents a workforce constraint that limits the scalability and effectiveness of programs. Moreover, the continuous need to adapt to evolving healthcare regulations, payer policies, and technology updates requires ongoing resource allocation, which can strain organizational capabilities and lead to implementation delays.
Significant opportunities within the CDI market are emerging from the integration of cutting-edge technologies like artificial intelligence (AI) and machine learning (ML), which promise to revolutionize documentation review and provider education. There is also considerable potential for market expansion into traditionally underserved segments such as ambulatory care settings, physician practices, and post-acute care facilities, as these areas increasingly fall under value-based care mandates and require improved data accuracy. CDI can also play a more central and proactive role in broader population health management strategies by ensuring the underlying data used for risk stratification and health outcome measurement is precise and reliable. The overall impact forces on the market are predominantly positive, with a growing recognition among healthcare leaders that CDI is not merely a compliance or revenue tool, but a critical strategic function essential for both financial sustainability and the delivery of high-quality, patient-centric care. This understanding is driving continued innovation and investment in the sector.
Segmentation Analysis
The Clinical Documentation Improvement (CDI) market is comprehensively segmented across various critical dimensions including product type, deployment model, end-user, and application. This granular segmentation provides a detailed understanding of the markets structure and allows for targeted analysis of specific industry dynamics. Product type typically differentiates between dedicated CDI software platforms, a range of CDI services encompassing consulting, education, and outsourcing, and integrated solutions that combine both technological and human expertise. Deployment models categorize offerings as either on-premise, providing greater control, or cloud-based, emphasizing flexibility and scalability. End-users span the entire healthcare spectrum, from large hospital systems to individual physician practices, each with unique needs and adoption drivers. Application-wise, CDI is foundational for enhancing quality reporting, ensuring robust compliance, optimizing revenue cycle management, and accurately supporting risk adjustment initiatives. Analyzing these segments is crucial for stakeholders to identify specific market niches, understand demand patterns, and strategically position their offerings within the evolving healthcare landscape.
- By Product Type:
- CDI Software Solutions (e.g., NLP-based platforms, analytics tools)
- CDI Services (e.g., Consulting, Outsourcing, Education & Training, Audit & Compliance)
- Integrated CDI Platforms (combining software and services)
- By Deployment Model:
- On-premise (requiring in-house infrastructure and IT management)
- Cloud-based (Software-as-a-Service, offering scalability and remote access)
- By End-User:
- Hospitals and Health Systems (Acute Care, Academic Medical Centers)
- Ambulatory Care Centers (Outpatient Clinics, Specialty Centers)
- Physician Practices and Groups
- Other Healthcare Providers (e.g., Long-Term Care Facilities, Skilled Nursing Facilities, Home Health Agencies)
- Healthcare Payers and Accountable Care Organizations (ACOs)
- By Application:
- Quality Reporting and Performance Metrics Improvement
- Regulatory Compliance and Audit Risk Mitigation
- Revenue Cycle Management and Reimbursement Optimization (e.g., DRG accuracy, CMI improvement)
- Risk Adjustment Documentation and Severity of Illness Capture
- Clinical Research, Data Analytics, and Public Health Initiatives
Clinical Documentation Improvement Market Value Chain Analysis
The value chain for the Clinical Documentation Improvement (CDI) market is intricate, commencing with upstream activities primarily centered on technology development and intellectual property creation. This segment involves specialized software vendors, AI and NLP solution providers, and content developers who build the foundational platforms, algorithms, and clinical knowledge bases that power CDI programs. These innovators are responsible for creating the sophisticated tools necessary for automated chart review, data extraction from unstructured notes, and real-time guidance systems. The quality and advancement of these core technological components significantly influence the effectiveness and efficiency of the entire CDI ecosystem. Investment in research and development at this stage is crucial for driving innovation and maintaining a competitive edge in a rapidly evolving market.
Midstream activities in the CDI value chain involve the delivery and implementation of these technologies and expertise to end-users. This segment includes CDI consulting firms that provide strategic guidance, program design, and ongoing optimization support. It also encompasses outsourcing service providers who offer skilled CDI professionals to healthcare organizations that may lack internal resources or prefer to offload the function. Furthermore, training and education providers are vital, ensuring that CDI specialists, coding professionals, and clinical staff are equipped with the latest knowledge and skills to effectively utilize CDI tools and adhere to documentation best practices. These intermediaries bridge the gap between technology creators and healthcare providers, facilitating the successful adoption and integration of CDI initiatives.
Downstream analysis focuses on the direct application of CDI within healthcare organizations and its impact on the final output – accurate, complete, and compliant medical records. This stage involves the day-to-day work of CDI specialists, coders, and clinicians who collaborate to review documentation, query physicians for clarification, and make necessary improvements. Distribution channels for CDI solutions are multifaceted; they include direct sales by software vendors to hospitals and health systems, partnerships with Electronic Health Record (EHR) providers for seamless integration, and indirect channels through healthcare IT consulting firms or value-added resellers. The interplay between these stages ensures that the technological solutions and expert services effectively reach the end-users, ultimately enhancing clinical data integrity, optimizing reimbursement, and supporting improved patient outcomes across the healthcare spectrum.
Clinical Documentation Improvement Market Potential Customers
The primary potential customers for Clinical Documentation Improvement (CDI) solutions are healthcare organizations burdened with the dual responsibility of delivering high-quality patient care and managing complex financial and regulatory landscapes. Hospitals and large integrated health systems represent the most significant segment of end-users. These institutions face intricate coding requirements, manage high patient volumes across diverse specialties, and are under constant pressure to optimize their revenue cycle while maintaining impeccable quality and compliance. For these organizations, CDI is not merely a tool for revenue enhancement but a strategic imperative for ensuring the integrity of their clinical data, which underpins everything from public quality reporting to long-term strategic planning. They seek comprehensive solutions that can integrate seamlessly with their existing Electronic Health Record (EHR) systems and provide actionable insights across their vast operations.
Beyond the acute care setting, ambulatory care centers and large physician practices are rapidly emerging as crucial potential customers for CDI. As value-based care models increasingly extend beyond inpatient environments, these outpatient facilities are recognizing the critical need for precise documentation to support risk adjustment, manage population health effectively, and accurately demonstrate performance against quality metrics. The shift towards outpatient care as a primary setting for chronic disease management and preventive services makes robust CDI indispensable for these providers to secure appropriate reimbursement and avoid penalties in performance-based payment programs. These customers typically require scalable, user-friendly solutions that can be easily integrated into their existing workflows without significant disruption.
Furthermore, healthcare payers and Accountable Care Organizations (ACOs) are demonstrating a growing interest in leveraging CDI to ensure the integrity and accuracy of the underlying clinical data used for risk stratification, provider profiling, and population health management. Accurate documentation directly impacts their financial models, their ability to appropriately manage patient populations, and their capacity to design effective incentive programs. While not direct implementers of CDI in the same way providers are, payers often invest in or promote CDI initiatives to their network providers to improve overall data quality across the healthcare ecosystem. Additionally, governmental health agencies and research institutions also stand as indirect beneficiaries and potential customers, as they rely on clean, complete clinical data for epidemiological studies, policy development, and public health initiatives, further broadening the scope of CDIs influence and potential customer base.
Clinical Documentation Improvement Market Key Technology Landscape
The Clinical Documentation Improvement (CDI) market is increasingly driven by a sophisticated and rapidly evolving technological landscape, designed to enhance the efficiency, accuracy, and comprehensiveness of clinical documentation. At the core of this landscape are advanced software platforms that leverage cutting-edge artificial intelligence (AI) and machine learning (ML) algorithms. These AI-powered tools are foundational for automating the meticulous review of unstructured clinical notes, a task traditionally performed manually by CDI specialists. Technologies like Natural Language Processing (NLP) are particularly crucial, as they enable systems to understand, interpret, and extract meaningful information from free-text clinical narratives, identifying potential documentation deficiencies, opportunities for clarification, and compliance risks in real-time. This automation significantly reduces the administrative burden, allowing CDI professionals to focus on higher-value tasks such as physician education and complex case analysis.
Robust integration capabilities with Electronic Health Record (EHR) systems are paramount within the CDI technology landscape. Seamless interoperability ensures that CDI insights and recommendations are embedded directly within the clinical workflow, providing immediate guidance to healthcare providers at the point of care. This direct integration facilitates prompt physician response to queries, reducing delays in documentation improvement and ultimately enhancing the overall quality and completeness of the patient record. Beyond EHR integration, the landscape also includes advanced data analytics and business intelligence platforms. These tools provide comprehensive dashboards and reports that track key CDI program metrics, identify trends in documentation errors, measure the financial impact of improved documentation, and highlight areas for targeted educational interventions. Such analytical capabilities are vital for continuous program optimization and demonstrating return on investment.
Further enhancing the technological framework are innovations such as secure cloud infrastructure, which enables scalable, flexible, and accessible CDI solutions, supporting remote workforces and distributed healthcare networks. Mobile applications are also gaining traction, offering convenient access to CDI tools and resources for clinicians and specialists on the go. Predictive analytics represents another significant advancement, allowing systems to anticipate potential documentation issues before they occur, based on historical data and patient profiles, thereby shifting CDI from a reactive to a proactive process. These technologies collectively aim to make CDI more intuitive, efficient, and deeply integrated into the daily operations of healthcare providers, ultimately fostering a culture of precise and comprehensive clinical documentation that supports both patient care excellence and organizational financial health.
Regional Highlights
- North America: Dominates the CDI market due to well-established healthcare infrastructure, stringent regulatory compliance mandates (e.g., ICD-10, MACRA, DRG systems), high adoption rates of EHRs, and a strong emphasis on value-based care models. The United States accounts for the largest share, driven by a complex reimbursement system and a proactive approach to revenue integrity and quality reporting. Canada also contributes significantly with its evolving healthcare policies.
- Europe: Exhibits significant growth, propelled by increasing healthcare expenditure, a concerted push towards digital transformation in healthcare, and the imperative to standardize clinical data across various national health systems. Countries like Germany, the UK, France, and the Nordic nations are leading adoption, focusing on improving patient outcomes, optimizing resource utilization, and ensuring financial sustainability within their public and private healthcare sectors.
- Asia-Pacific: Poised for rapid expansion, fueled by rising awareness of CDI benefits, growing investment in healthcare infrastructure modernization, increasing adoption of advanced healthcare technologies, and a large, aging patient population base. Emerging economies such as China and India, alongside developed markets like Japan and Australia, are key contributors to market growth as they seek to enhance healthcare quality, efficiency, and financial performance.
- Latin America: Demonstrates nascent but accelerating growth, with increasing efforts across the region to improve healthcare quality, enhance operational efficiency, and adopt more sophisticated reimbursement methodologies. Governments and private healthcare providers are gradually adopting CDI solutions to address evolving regulatory environments, improve data accuracy, and align with international standards. Brazil and Mexico are showing particular interest.
- Middle East & Africa: Shows considerable potential, particularly within the Gulf Cooperation Council (GCC) countries, driven by significant government spending on healthcare infrastructure development, a strong focus on medical tourism, and a proactive approach to adopting international best practices for clinical documentation, patient safety, and revenue cycle management. Increasing digital literacy and investment in healthcare IT further support this growth.
Top Key Players
The market research report includes a detailed profile of leading stakeholders in the Clinical Documentation Improvement Market.- 3M Company
- Optum (UnitedHealth Group)
- Nuance Communications (Microsoft)
- Clinical Computer Systems, Inc. (Meditech)
- Guidehouse (acquired Navigant Consulting)
- Enjoin
- Craneware PLC
- Streamline Health Solutions, Inc.
- HIMagine Solutions
- CDI Partners
- YES HIM Consulting
- Iodine Software
- Health Language (part of Wolters Kluwer)
- Cotiviti
Frequently Asked Questions
What is Clinical Documentation Improvement (CDI) and why is it important?
Clinical Documentation Improvement (CDI) is a specialized process within healthcare designed to enhance the accuracy, completeness, and consistency of clinical documentation in patient medical records. It is critically important because precise documentation directly influences healthcare quality reporting, ensures patient safety, optimizes appropriate reimbursement, and facilitates robust compliance with a myriad of regulatory standards, ultimately ensuring that the care delivered is accurately reflected and appropriately compensated.
How does CDI impact healthcare revenue cycles?
CDI significantly impacts healthcare revenue cycles by ensuring that clinical documentation accurately reflects the patients true severity of illness, comorbidities, and the complexity of care provided. This precision leads to more accurate and defensible medical coding (e.g., DRG assignment, CMI enhancement), which in turn optimizes legitimate reimbursement from payers, substantially reduces claim denials, and effectively mitigates potential audit risks, thereby enhancing the financial health and sustainability of healthcare organizations.
What role does technology, particularly AI, play in CDI?
Technology, especially Artificial Intelligence (AI) and Natural Language Processing (NLP), plays a transformative role in CDI by automating the initial chart review process, intelligently identifying potential documentation deficiencies in real-time, and providing proactive, context-sensitive prompts to clinicians. AI enhances operational efficiency, improves the accuracy and completeness of records, and allows human CDI specialists to dedicate their expertise to more complex cases and critical provider education, thereby streamlining the entire documentation workflow.
Who typically benefits from implementing a CDI program?
The primary beneficiaries of comprehensive CDI programs are hospitals, large health systems, ambulatory care centers, and physician practices, as well as healthcare payers and Accountable Care Organizations (ACOs). These entities benefit from enhanced revenue integrity, improved quality scores, reduced compliance and audit risks, more accurate data for clinical analytics, and robust population health management, leading to overall improvements in operational efficiency and clinical outcomes.
What are the main challenges in implementing a successful CDI program?
Key challenges in establishing and sustaining an effective CDI program include achieving consistent and enthusiastic physician engagement and buy-in, overcoming the significant initial investment required for advanced technology and comprehensive staff training, addressing the scarcity of experienced and dually credentialed CDI professionals, and continuously adapting to the rapidly evolving landscape of healthcare regulations, coding standards, and payer policies. These hurdles necessitate strong leadership, strategic planning, and ongoing education.
To check our Table of Contents, please mail us at: sales@marketresearchupdate.com
Research Methodology
The Market Research Update offers technology-driven solutions and its full integration in the research process to be skilled at every step. We use diverse assets to produce the best results for our clients. The success of a research project is completely reliant on the research process adopted by the company. Market Research Update assists its clients to recognize opportunities by examining the global market and offering economic insights. We are proud of our extensive coverage that encompasses the understanding of numerous major industry domains.
Market Research Update provide consistency in our research report, also we provide on the part of the analysis of forecast across a gamut of coverage geographies and coverage. The research teams carry out primary and secondary research to implement and design the data collection procedure. The research team then analyzes data about the latest trends and major issues in reference to each industry and country. This helps to determine the anticipated market-related procedures in the future. The company offers technology-driven solutions and its full incorporation in the research method to be skilled at each step.
The Company's Research Process Has the Following Advantages:
- Information Procurement
The step comprises the procurement of market-related information or data via different methodologies & sources.
- Information Investigation
This step comprises the mapping and investigation of all the information procured from the earlier step. It also includes the analysis of data differences observed across numerous data sources.
- Highly Authentic Source
We offer highly authentic information from numerous sources. To fulfills the client’s requirement.
- Market Formulation
This step entails the placement of data points at suitable market spaces in an effort to assume possible conclusions. Analyst viewpoint and subject matter specialist based examining the form of market sizing also plays an essential role in this step.
- Validation & Publishing of Information
Validation is a significant step in the procedure. Validation via an intricately designed procedure assists us to conclude data-points to be used for final calculations.
×
Request Free Sample:
Related Reports
Select License

Why Choose Us

We're cost-effective and Offered Best services:
We are flexible and responsive startup research firm. We adapt as your research requires change, with cost-effectiveness and highly researched report that larger companies can't match.

Information Safety
Market Research Update ensure that we deliver best reports. We care about the confidential and personal information quality, safety, of reports. We use Authorize secure payment process.

We Are Committed to Quality and Deadlines
We offer quality of reports within deadlines. We've worked hard to find the best ways to offer our customers results-oriented and process driven consulting services.

Our Remarkable Track Record
We concentrate on developing lasting and strong client relationship. At present, we hold numerous preferred relationships with industry leading firms that have relied on us constantly for their research requirements.

Best Service Assured
Buy reports from our executives that best suits your need and helps you stay ahead of the competition.

Customized Research Reports
Our research services are custom-made especially to you and your firm in order to discover practical growth recommendations and strategies. We don't stick to a one size fits all strategy. We appreciate that your business has particular research necessities.

Service Assurance
At Market Research Update, we are dedicated to offer the best probable recommendations and service to all our clients. You will be able to speak to experienced analyst who will be aware of your research requirements precisely.
Contact With Our Sales Team
Customer Testimonials
The content of the report is always up to the mark. Good to see speakers from expertise authorities.
Privacy requested , Managing Director
A lot of unique and interesting topics which are described in good manner.
Privacy requested, President
Well researched, expertise analysts, well organized, concrete and current topics delivered in time.
Privacy requested, Development Manager