Telehealth Services Market Size By Region (North America, Europe, Asia-Pacific, Latin America, Middle East and Africa), By Statistics, Trends, Outlook and Forecast 2025 to 2032 (Financial Impact Analysis)
ID : MRU_ 429040 | Date : Oct, 2025 | Pages : 249 | Region : Global | Publisher : MRU
Telehealth Services Market Size
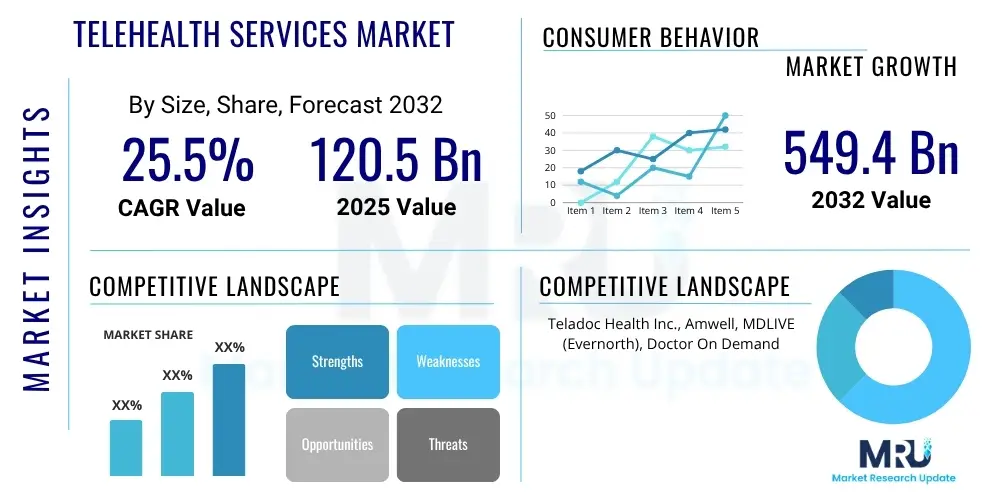
The Telehealth Services Market is projected to grow at a Compound Annual Growth Rate (CAGR) of 25.5% between 2025 and 2032. The market is estimated at $120.5 Billion in 2025 and is projected to reach $549.4 Billion by the end of the forecast period in 2032.
Telehealth Services Market introduction
Telehealth services encompass a broad range of healthcare activities delivered remotely using information and communication technologies. This includes virtual consultations, remote patient monitoring (RPM), mobile health (mHealth), and digital transmission of medical images and data. These services enable patients to access medical care from the comfort of their homes, reducing geographical barriers and wait times. Major applications span primary care, chronic disease management, mental health support, specialist consultations, and emergency services triage. The primary benefits include enhanced accessibility to healthcare, particularly for underserved populations, significant cost efficiencies for both patients and providers, and improved patient convenience. The market's growth is predominantly driven by increasing smartphone penetration, the rising prevalence of chronic diseases, a global shortage of healthcare professionals, and supportive government initiatives promoting digital health solutions.
Telehealth Services Market Executive Summary
The telehealth services market is experiencing dynamic expansion, shaped by several key trends. Business trends highlight a strong move towards integrated hybrid care models combining in-person and virtual visits, significant investment in platform interoperability, and the increasing adoption of AI and machine learning to enhance diagnostics and operational efficiency. Regionally, North America and Europe continue to lead in adoption due to established infrastructure and favorable regulatory environments, while Asia Pacific is emerging as the fastest-growing market driven by vast populations, increasing digital literacy, and improving internet connectivity. In terms of segments, virtual visits remain the largest contributor, but remote patient monitoring (RPM) is poised for accelerated growth, fueled by the rising burden of chronic conditions and advancements in wearable technologies. The market is also seeing a diversification into specialized telehealth services, moving beyond general consultations to address specific clinical needs like tele-dermatology, tele-ophthalmology, and tele-psychiatry.
AI Impact Analysis on Telehealth Services Market
User questions regarding AI's impact on telehealth frequently center on its ability to enhance diagnostic accuracy, personalize patient care, and streamline operational workflows. There is significant interest in how AI can support clinicians, predict health outcomes, and improve accessibility to care, particularly in remote areas. Users also express concerns about data privacy, algorithmic bias, and the ethical implications of AI-driven healthcare decisions. The general expectation is that AI will transform telehealth by making services more efficient, precise, and tailored to individual patient needs, while also addressing challenges related to data management and clinical decision support. This integration is seen as crucial for scaling telehealth services and enhancing their overall effectiveness, moving beyond basic video consultations to more sophisticated and data-driven interventions.
- AI-powered diagnostic tools improve accuracy in image analysis and symptom assessment.
- Predictive analytics identify at-risk patients for proactive intervention and personalized care plans.
- Automated chatbots and virtual assistants enhance patient engagement and initial triage.
- Operational efficiency gains through AI-driven scheduling, billing, and administrative tasks.
- Enhanced data analysis for better understanding of population health trends and treatment efficacy.
- Development of personalized treatment pathways based on individual patient data.
- Fraud detection and security enhancements through AI-driven anomaly detection.
DRO & Impact Forces Of Telehealth Services Market
The telehealth services market is propelled by a confluence of powerful drivers, tempered by specific restraints, and ripe with opportunities, all contributing to its dynamic impact forces. Key drivers include the overwhelming convenience and cost-effectiveness offered to patients, the increasing burden of chronic diseases necessitating continuous monitoring, and the persistent shortage of healthcare professionals globally, making remote care a viable solution. Furthermore, the indelible legacy of the COVID-19 pandemic significantly accelerated adoption, alongside growing governmental support and favorable reimbursement policies. However, significant restraints challenge market expansion, notably the complex and often fragmented regulatory landscape across different regions, critical concerns around data security and patient privacy, and the 'digital divide' impacting access for elderly or technologically disadvantaged populations. The lack of standardized reimbursement models and resistance from traditional healthcare providers also pose hurdles. Amidst these, vast opportunities emerge, particularly in the integration of artificial intelligence for advanced diagnostics and personalized medicine, expansion into underserved rural and remote areas, and a dedicated focus on mental health services. The evolution towards hybrid care models, blending virtual and in-person care, further defines the market's trajectory. These interplay of forces collectively shape the market's growth, innovation, and strategic direction.
Segmentation Analysis
The telehealth services market is comprehensively segmented across various dimensions to provide a nuanced understanding of its intricate structure and growth avenues. These segments delineate the diverse offerings, applications, and end-user adoption patterns that define the market landscape. The primary segmentation categories include service type, application, end-use, and component, each revealing distinct market dynamics and investment opportunities. Understanding these segments is crucial for market participants to tailor their strategies, develop targeted solutions, and address specific demands within the evolving healthcare ecosystem. The rapid technological advancements and shifting patient expectations further influence the growth and prominence of these segments, making continuous analysis essential for strategic planning.
- By Service Type:
- Real-time (Synchronous)
- Video Conferencing
- Audio Consultations
- Store-and-forward (Asynchronous)
- Image and Data Transmission
- Secure Messaging
- Remote Patient Monitoring (RPM)
- Physiological Monitoring
- Wearable Devices
- mHealth
- Real-time (Synchronous)
- By Application:
- Radiology
- Teleradiology
- Cardiology
- Telecardiology
- Primary Care
- Mental Health
- Telepsychiatry
- Telepsychology
- Dermatology
- Teledermatology
- Pathology
- Telepathology
- Emergency Services
- Others (e.g., Teleneurology, Teleophthalmology)
- Radiology
- By End-Use:
- Providers
- Hospitals
- Clinics
- Physician Groups
- Payers
- Insurance Companies
- Government Agencies
- Patients
- Employers and Businesses
- Providers
- By Component:
- Software
- Standalone Solutions
- Integrated Platforms
- Hardware
- Monitors
- Medical Peripherals
- Kiosks
- Services
- Consulting
- Implementation
- Training
- Maintenance
- Software
Value Chain Analysis For Telehealth Services Market
The value chain for the telehealth services market encompasses a sophisticated network of interconnected stages, from initial technology development to direct patient care, highlighting the flow of value creation. Upstream activities involve technology providers specializing in hardware (e.g., remote monitoring devices, cameras) and software (e.g., virtual consultation platforms, EHR integration, AI analytics), alongside content creators developing educational and therapeutic materials. Midstream, service aggregators and platform developers integrate these technologies, ensuring interoperability and a seamless user experience. Downstream, the distribution channels are multifaceted, including direct-to-consumer platforms, B2B partnerships with hospitals and clinics, and collaborations with insurance companies and employers for wellness programs. Patients are the ultimate beneficiaries, directly accessing care, while healthcare providers act as critical intermediaries. The market involves both direct provision of services from telehealth companies to consumers and indirect delivery through established healthcare networks, emphasizing diverse engagement models.
Telehealth Services Market Potential Customers
The potential customers for telehealth services are highly diverse, encompassing a broad spectrum of individuals and entities within the healthcare ecosystem. At the forefront are individual patients, particularly those residing in rural or underserved areas, individuals with mobility challenges, elderly populations, and those managing chronic conditions requiring frequent monitoring. Furthermore, patients seeking convenient access to specialized care, mental health support, or routine primary care represent a significant customer base. Beyond individual patients, healthcare providers such as hospitals, urgent care centers, primary care clinics, and large physician groups are key institutional buyers, leveraging telehealth to expand reach, improve efficiency, and manage patient flow. Insurance companies and government health agencies also stand as crucial customers, as they integrate telehealth into their coverage plans to enhance population health management and reduce healthcare costs. Lastly, employers increasingly offer telehealth as part of their employee wellness programs, recognizing its benefits in improving employee health and productivity.
| Report Attributes | Report Details |
|---|---|
| Market Size in 2025 | $120.5 Billion |
| Market Forecast in 2032 | $549.4 Billion |
| Growth Rate | 25.5% CAGR |
| Historical Year | 2019 to 2023 |
| Base Year | 2024 |
| Forecast Year | 2025 - 2032 |
| DRO & Impact Forces |
|
| Segments Covered |
|
| Key Companies Covered | Teladoc Health Inc., Amwell, MDLIVE (Evernorth), Doctor On Demand (Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in Included in In
To check our Table of Contents, please mail us at: sales@marketresearchupdate.com
Research Methodology The Market Research Update offers technology-driven solutions and its full integration in the research process to be skilled at every step. We use diverse assets to produce the best results for our clients. The success of a research project is completely reliant on the research process adopted by the company. Market Research Update assists its clients to recognize opportunities by examining the global market and offering economic insights. We are proud of our extensive coverage that encompasses the understanding of numerous major industry domains. Market Research Update provide consistency in our research report, also we provide on the part of the analysis of forecast across a gamut of coverage geographies and coverage. The research teams carry out primary and secondary research to implement and design the data collection procedure. The research team then analyzes data about the latest trends and major issues in reference to each industry and country. This helps to determine the anticipated market-related procedures in the future. The company offers technology-driven solutions and its full incorporation in the research method to be skilled at each step. The Company's Research Process Has the Following Advantages:
The step comprises the procurement of market-related information or data via different methodologies & sources.
This step comprises the mapping and investigation of all the information procured from the earlier step. It also includes the analysis of data differences observed across numerous data sources.
We offer highly authentic information from numerous sources. To fulfills the client’s requirement.
This step entails the placement of data points at suitable market spaces in an effort to assume possible conclusions. Analyst viewpoint and subject matter specialist based examining the form of market sizing also plays an essential role in this step.
Validation is a significant step in the procedure. Validation via an intricately designed procedure assists us to conclude data-points to be used for final calculations.
×
Request Free Sample:Related Reports
Select License
 Why Choose Us
 We're cost-effective and Offered Best services:We are flexible and responsive startup research firm. We adapt as your research requires change, with cost-effectiveness and highly researched report that larger companies can't match.  Information SafetyMarket Research Update ensure that we deliver best reports. We care about the confidential and personal information quality, safety, of reports. We use Authorize secure payment process.  We Are Committed to Quality and DeadlinesWe offer quality of reports within deadlines. We've worked hard to find the best ways to offer our customers results-oriented and process driven consulting services.  Our Remarkable Track RecordWe concentrate on developing lasting and strong client relationship. At present, we hold numerous preferred relationships with industry leading firms that have relied on us constantly for their research requirements.  Best Service AssuredBuy reports from our executives that best suits your need and helps you stay ahead of the competition.  Customized Research ReportsOur research services are custom-made especially to you and your firm in order to discover practical growth recommendations and strategies. We don't stick to a one size fits all strategy. We appreciate that your business has particular research necessities.  Service AssuranceAt Market Research Update, we are dedicated to offer the best probable recommendations and service to all our clients. You will be able to speak to experienced analyst who will be aware of your research requirements precisely. Contact With Our Sales Team
Customer Testimonials
The content of the report is always up to the mark. Good to see speakers from expertise authorities. Privacy requested , Managing Director A lot of unique and interesting topics which are described in good manner. Privacy requested, President Well researched, expertise analysts, well organized, concrete and current topics delivered in time. Privacy requested, Development Manager Our ClientsAbout usMarket Research Update is market research company that perform demand of large corporations, research agencies, and others. We offer several services that are designed mostly for Healthcare, IT, and CMFE domains, a key contribution of which is customer experience research. We also customized research reports, syndicated research reports, and consulting services. Usefull LinksContact UsMarket Research UpdateIndia : Office no - 406, 4th floor, Suratwala Mark Plazzo, Hinjewadi, Pune 411057 Japan: 16-8, Higashi 1-chome, Shibuya-ku, Tokyo 150-0011, Japan (UK) +1-252-552-1404 sales@marketresearchupdate.com SUBSCRIBEGet the latest news and insights from MRU delivered to your inbox Trust Online
|